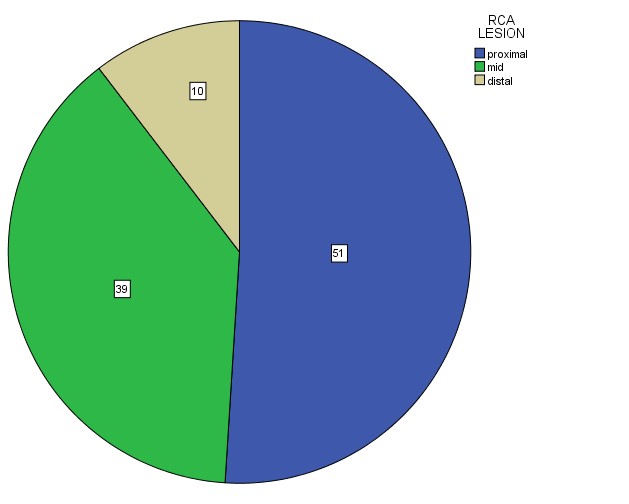
The presents study aimed at predicting the site of lesion in RCA by measuring the height of ST Segment elevation included a total of 50 patients of acute inferior MI. With the help of 12-lead ECG, magnitudes of ST-seginent elevation in leads II, III and aVF were measured. The highest degree of stenosis along the RCA revealed by angiograms was accepted as the culprit lesion. Right coronary artery was divided into proximal (from its ostium to the origin of RV branch), mid (from the RV branch to the acute marginal branch) and distal (from the acute marginal branch onward) parts. The sum of ST segment elevation was then computed and compared among the three groups of patients divided on the basis of site of lesion in RCA. The findings obtained from data analyses are documented below.
Demographic characteristics:
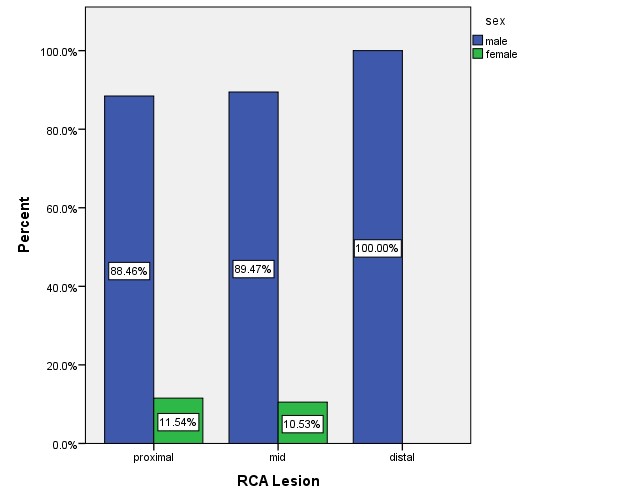
Table I demonstrates the distribution of demographic characteristics among the three groups. The age distribution was almost homogeneous among the three groups (F =0.069, p =0.933). Males were predominant among the groups (x2 =0.630, p =0.730).
Table I. Demographic characteristics among the three groups
|
Demographic characteristics |
RCA Lesion
|
p-value | ||
| Proximal
(n = 26) |
Mid
(n= 19) |
Distal
(n = 05) |
||
| Age (year)# | 54.6 ±5.2 | 54.6 ± 5.9 | 55.6 ± 4.4 | 0.933 |
| Sex¶
Male Female |
23(88.5)
03(11.5) |
17(89.5)
02(10.5) |
05(100.0)
00(00) |
0.730 |
# Data were analyzed using ANOVA statistics and are presented as mean ± SD;
¶ Data were analyzed using x2 Test.
Figures in the parentheses denote corresponding percentage.
Clinical presentation & examination:
The mean duration of chest pain was almost similar among the three groups (F = 3.046, p = 0.057). There was no significant difference in pulse rate among the groups (F =0.811, p =0.450). The mean systolic and diastolic blood pressures were significantly higher in the distal group than those in proximal and mid groups (F =7.983, p =0.001 and F =3.480, p=0.039 respectively). The proportion of patients with shortness of breath, sweating and nausea were significantly higher in the proximal group than those in other two groups; however vomiting was found identically distributed among the groups (x2 =8.864, p =0.012; x2 =13.543, p =0.001; x2 =10.499, p =0.005; x2 =3.338 p =0.188) (Table II).
Table II. Clinical presentation & examination among the three groups
|
Clinical presentations & Examination |
RCA Lesion
|
p-value | ||
| Proximal
(n = 26) |
Mid
(n = 19) |
Distal
(n = 05) |
||
| Duration of chest pain#
(hours) Pulse (beats/mm) # Systolic BP (mm of hg) # Diastolic BP(mm of Hg) #
Shortness of breath¶ Yes No Sweating¶ Yes No Nausea¶ Yes No Vomiting¶ Yes No |
7.0±1.16
72.8± 5.29 109 ± 11 73 ± 9 19(73.1) 7(26.9) 20 (76.9) 6(23.1) 16(61.5) 10(38.5) 14(53.8) 12(46.2) |
7.74±0.73
75.4± 12.5 118± 17 82 ± 16 6(31.6) 13(68.9) 5(26.3) 14(73.7) 3(15.8) 16(84.2) 6(31.6) 13(68.4) |
7.60±1.14
77.2±4.1 136± 18 82± 12 4(80.0) 1(20.0) 1(20.0) 4(80.0) 1(20.0) 4(80.0) 1(20.0) 4(80.0) |
0.057
0.450 0.001 0.039 0.012 0.001 0.005 0.188 |
#Data were analyzed using ANOVA statistics and are presented as mean ± SD;
¶Data were analyzed using x2 Test.; figures in parentheses denote corresponding %.
7.3 Cardiovascular risk factors:
Table III shows that smoking habit, diabetes and dyslipidemia were significantly higher in the proximal group than those in mid and distal group (x =7.798, p =0.020; x2 =6.826, p =0.033 and x2 =10.499, p =0.005 respectively). Hypertension and family history of IHD were also higher in proximal group than those in other two groups, although the difference did not turn to significant (x2 =2.451, p =0.294 and x2 =0.685, p =0.710 respectively).
Table III. Cardiovascular risk factors among the three groups
|
Risk factors¶ |
RCA Lesion
|
p-value | ||
| Proximal
(n = 26) |
Mid
(n = 19) |
Distal
(n = 05) |
||
| Smoking habit
Yes No DM Yes No HTN Yes No Dyslipidaemia Yes No Family H/O IHD Yes No |
21(80.8)
5(19.2) 16(61.5) 10(38.5) 17(65.4) 9(34.6) 16(61.5) 10(38.5) 5(19.2) 21(80.8) |
8(42.1)
11(57.9) 05(26.31) 14(73.68) 8(42.1) 11(57.9) 3(15.8) 16(84.2) 2(10.5) 17(89.5) |
4(80.0)
1(20.0) 1(20.0) 3(80.0) 3(60.0) 2(40.0) 1(20.0) 4(80.0) 1(20.0) 4(80.0) |
0.020
0.033 0.294 0.005 0.710 |
¶ Data were analyzed using x2 Test.
Figures in the parentheses denote corresponding percentage.
In-hospital complications:
Approximately three quarter (73.1%) of the patients in proximal group experienced hypotension,46.2% cardiogenic shock, 42.3% acute LVF and 46.2% arrhythmias. In mid group, about 15.8% of the patients had hypotension, 10.5% cardiogenic shock, 10.5% acute LVF and another 10.5% arrhythmias. 40% of patients in distal group had hypotension and 20% arrhythmias. All the in-hospital complications were observed to be significantly higher in the proximal group than those in other two groups (x2 =14.577, p =0.001; x2 =9.072, p =0.011; x2 =7.715, p =0.021; x2 =6.900, p=0.032) (Table IV).
Table IV. In-hospital complications among the three groups
|
Complications¶ |
RCA Lesion
|
p-value | ||
| Proximal
(n = 26) |
Mid
(n = 19) |
Distal
(n = 05) |
||
| Hypotension
Yes No Cardiogenic shock Yes No Acute LVF Yes No Arrhythmia Yes No |
19(73.1)
7(26.9) 12(46.2) 14(53.8) 11(42.3) 15(57.7) 12(46.2) 14(53.8) |
3(15.8)
16(84.2) 2(10.5) 17(89.5) 2(10.5) 17(89.5) 2(10.5) 17(89.5) |
1(20.0)
4(80.0) 0(0.0) 5(100.0) 0(0.0) 5(100.0) 1(20.0) 4(80.0) |
0.001
0.011 0.021 0.032 |
¶ Data were analyzed using x2 Test.
Figures in the parentheses denote corresponding percentage.
Echocardiograpnic findings:
Echocardiographic findings demonstrate that 20(76.9%) of 26 patients had regional wall motion abnormality (RWMA) in inferior wall in proximal group, 52.6% in mid group and 20% distal group (x =6.909, p=0.032). The mean percentage of left ventricular ejection fraction failure (LVEF) of proximal group had ( 45.67 ± 11.96), (49.31 ± 10.15) in mid and (57.28 ± 7.66) in distal group (F =2.493, p=0.094)
(Table V).
Table V. Echocardiogram among the three groups
| Echocardiogram RCA Lesion | ||||
| Proximal
(n = 26) |
Mid
(n = 19) |
Distal
(n = 05) |
p-value | |
| RWMA¶
Yes No LVEF(%) |
20(76.9)
6(23.1) 45.67±11.96 |
10(52.6)
09(47.4) 49.31±10.15 |
1(20.0)
4(80.0) 57.28±7.66 |
0.032
0.094 |
¶Data were analyzed using x2 Test.
#Data were analyzed using ANOVA statistics and are presented as mean ± SD.
Note: In this study LV EF(%) were observed by echocardiography. As in this study among the acute inferior myocardial infarction 30% patient had RVI so measurement of RV EF might be more representative.
Association of RVI with site of lesion in RCA:
More than half (53.8%) of the proximal lesions and 5.3% of the mid lesions in
RCA had RVI. None of the distal lesions had RVI.
Table VI. Association of RVI with site of lesion in RCA
| RCA Lesion | ||||
| RVI | Proximal
(n = 26) |
Mid
(n = 19) |
Distal
(n = 05) |
p-value |
| Present
Absent |
14(53.8)
12(46.2) |
1(5.3)
18(94.7) |
0(0.0)
5(100.0) |
0.001 |
¶ Data were analyzed using Chi-square (x2) Test.
Figures in the parentheses denote corresponding percentage.
ST segment elevation and site of lesion in RCA
The mean heights of ST-segment elevation in Lead II, Lead III and aVF and the
sum of ST-segment elevation showed a decreasing trend with progress of lesion
from proximal to distal site of RCA (F=78.660, p=0.000; F =87.123 p=0.000; F=34.438, p=0.000; F=157.747, p=0.000) (Table VII & Fig. 5).
Table VII. Association of ST segment elevation with site of lesion in RCA
| ST segment elevatio # RCA
(mm) |
||||
| Proximal
(n = 48) |
Mid
(n = 38) |
Distal
(n = 14) |
p-value | |
| Lead II
Lead III aVF sum of ST segment elevation |
3.42 ± 0.42
4.83 ± 0.39 4.26 ± 0.85 12.52 ± 1.07 |
2.11 ± 0.44
3.60 ± 0.43 2.83 ± 0.45 8.54 ± 0.80 |
1.35 ± 0.45
2.60 ± 0.5 2.17 ± 0.24 6.15 ± 0.42 |
<0.001
<0.001 <0.001 <0.001 |
#Data were analyzed using ANOVA statistics and are presented as mean ± SD;
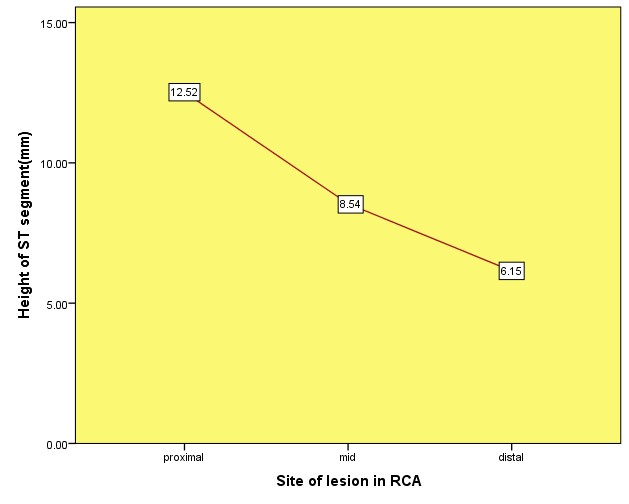 Showing relationship of height of ST elevation with site of lesion in RCA
Showing relationship of height of ST elevation with site of lesion in RCA
Charts: